Chapter Thirteen Meaning and Application of Urine Chemistries
References
JC mentioned that the diagnostic accuracy of 24 hour urine collection increases with more collections! Metabolic evaluation of patients with recurrent idiopathic calcium nephrolithiasis
We didn't refer to a particular study on sodium intake and the 24 hour urine but this meta-analysis Comparison of 24‐hour urine and 24‐hour diet recall for estimating dietary sodium intake in populations: A systematic review and meta‐analysis - PMC 24‐hour diet recall underestimated population mean sodium intake.
Anna looking up ace i and urinary sodium Effects of ACE inhibition on proximal tubule sodium transport | American Journal of Physiology-Renal Physiology
The original FENa paper by Espinel: The FeNa Test: Use in the Differential Diagnosis of Acute Renal Failure | JAMA | JAMA Network
Schreir’s replication and expansion of Espinel’s data: Urinary diagnostic indices in acute renal failure: a prospective study
Here’s a report from our own JC on the Diagnostic Utility of Serial Microscopic Examination of the Urinary Sediment in Acute Kidney Injury | American Society of Nephrology
JC shared his journey regarding FENa and refers to his recent paper Concomitant Identification of Muddy Brown Granular Casts and Low Fractional Excretion of Urinary Sodium in AKI
And Melanie’s accompanying editorial Mind the Cast: FENa versus Microscopy in AKI : Kidney360 (with a great image from Samir Parikh)
JC referenced this study from Schrier on FENa with a larger series: Urinary diagnostic indices in acute renal failure: a prospective study
A classic favorite: Acute renal success. The unexpected logic of oliguria in acute renal failure
Marathon runners had granular casts in their urine without renal failure. Kidney Injury and Repair Biomarkers in Marathon Runners
Cute piece from Rick Sterns on urine electrolytes! Managing electrolyte disorders: order a basic urine metabolic panel
The Urine Anion Gap: Common Misconceptions | American Society of Nephrology
Excellent review from Halperin on urine chemistries (including some consideration of the TTKG): Use of Urine Electrolytes and Urine Osmolality in the Clinical Diagnosis of Fluid, Electrolytes, and Acid-Base Disorders - Kidney International Reports
Renal tubular acidosis (RTA): Recognize The Ammonium defect and pHorget the urine pH | SpringerLink
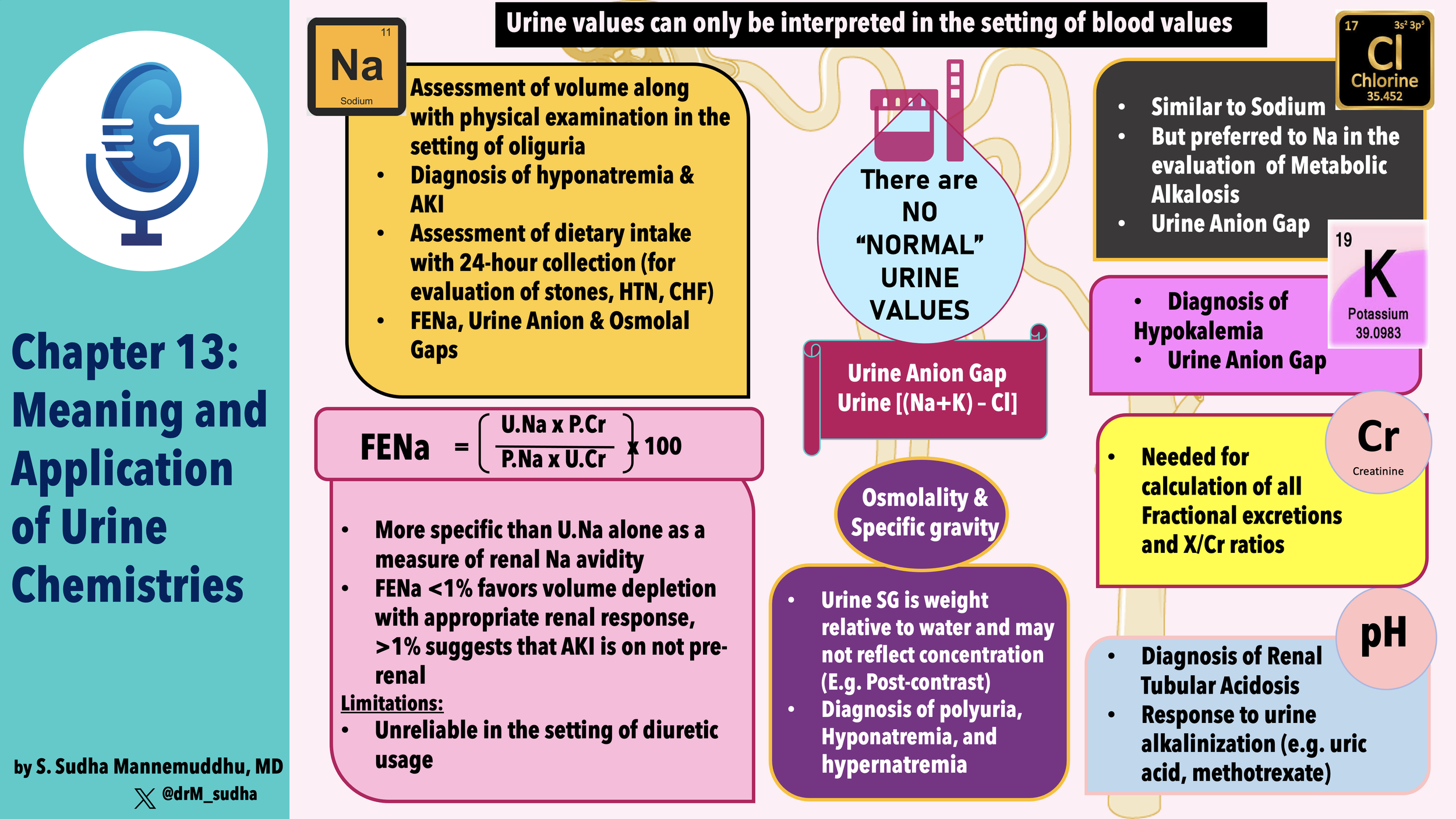
Outline
Chapter 13
- New part: Part 3, Physiologic approach to acid-base and electrolyte disorders
- Do you remember the previous two parts?
- Renal physiology
- Regulation of water and electrolyte balance
- Chapter 13: Meaning and application of urine chemistries
- Measurement of urinary electrolyte concentrations, osmolality and pH helps diagnose some conditions
- There are no fixed normal values
- Kidney varies rate of excretion to match intake and endogenous production
- Example: urine Na of 125/day can be normal if patient euvolemic on a normal diet, and wildly inappropriate in a patient who is volume depleted.
- Urine chemistries are:
- Useful
- Simple
- Widely available
- Usually a random sample is adequate
- 24-hour samples give additional context
- Gives example of urinary potassium, with extra renal loss of K, urine K should be < 25, but if the patient has concurrent volume deficiency and urine output is only 500 mL, then urine K concentration can appropriately be as high as 40 mEq/L
- Table 13-1
- Seems incomplete, see my notes on page 406
- What is Gravity ARF?
- Sodium Excretion
- Kidney varies Na to maintain effective circulating volume (I’d say volume homeostasis)
- Urine Na affected by RAAS and ANP
- Na concentration can be used to determine volume status
- Urine Na < 20 is hypovolemia
- Says it is especially helpful in determining the etiology of hyponatremia
- Calls out SIADH and volume depletion
- Used 40 mEq/L for SIADH
- Also useful in AKI
- Where differential is pre-renal vs ATN
- In addition to urine Na (and FENa) look at urine osmolality
- Again uses 40 mEq/l
- Mentions FENa and urine osmolality
- Urine Na can estimate dietary sodium intake
- Suggests doing this during treatment of hypertension to assure dietary compliance
- 24 hour urine Na is accurate with diuretics as long as the dose is stable and the drugs are chronic
- Diuretics increase Na resorption in other segments of the tubule that are not affected by the diuretic
- Points to increased AT2 induced proximal Na resorption and aldosterone induced DCT resoprtion
- In HTN shoot for less than 100 mEq/Day
- Urine Na useful in stones
- Urine uric acid and urine Ca can cause stones and their handling is dependent on sodium
- Low sodium diet can mask elevated excretion of these stone forming metabolites
- 24-hour Na > 75 and should be enough sodium to avoid this pitfall
- Pitfalls
- Low urine sodium in bilateral renal artery stenosis or acute GN
- High urine sodium with diuretics, aldo deficiency, advanced CKD
- Altered water handling can also disrupt this
- DI with 10 liters of urine and urine sodium excretion of 100 mEq is 10 mEq/L but in this case there is no volume deficiency
- Opposite also important, a lot of water resorption can mask volume deficiency by jacking up the urine sodium
- Advises you to use the FENa
- THE FENA
- < 1% dry
- >2-3% ATN
- It will fail with chronic effective volume depletion
- Heart failure, cirrhosis, and burns
- Suggests that tubular function will be preserved in those situations
- Also with contrast, rhabdo, pigment nephropathy
- Limitations
- Dependent on the amount of Na filtered
- Goes through the math of a normal person with GFR of 125/min and Na of 150 has filtered sodium of 27,000/day so if they eat 125-250 mEq their FENa will be <1%
- Talks about diuretics
- Can use FE lithium
- Mainly reabsorbed in the proximal tubule
- Not affected by loop diuretics
- 20% in healthy controls
- <15% in pre-renal disease
- Can use FE Uric acid
- Also not affected by loop diuretics
- Below 12% is pre-renal
- No FEUrea
- Chloride excretion
- Urine Cl and Na usually move in parallel
- However as many as 30% of hypovolemic patients have more than a 15 mEq/L difference between urine Na and Cl
- Due to Na excretion with another anion, HCO3 or carbenicillin or Cl with another cation, NH4+
- Discusses the metabolic alkalosis issue
- Says the urine Na can be over 100 in volume depleted patients with metabolic alkalosis!
- In metabolic acidosis (normal anion gap)
- Urine Cl should rise to balance out the NH4
- RTA should also have urine pH > 5.3
- Potassium excretion
- Can go as low at 5-25/day
- Low in extra renal losses
- Or after the diuretics have worn off
- More than 25/day indicates renal losses
- Not so helpful in hyperkalemia since chronic hyperkalemia is always due to a defect renal potassium excretion
- Expect always to have inappropriately low K with hyperkalemia due to
- Renal failure
- Hypoaldo
- Urine osmolality
- In hyponatremia it should < 100
- Hyponatremia here should be due to excessive water intake
- In hypernatremia it should be > 600-800
- Urine osm < plasma osm in face of hypernatremia indicates renal water loss due to lack of or resistance to ADH
- In ATN urine OSM < 400
- In pre-renal disease it could be over 500
- Specific but not sensitive due to people with CKD who are unable to concentrate urine
- Specific gravity
- Plasma is 8-10% igher than plasma so specific gravity is 1.008 to 1.010
- Every 30-35 mOsm/L raises urine Osm of 0.001
- so 1.010 is 300-350 mOsm/L H2O
- Glucose raises urine specific gravity more than osmolality
- Same with contrast
- Carbenicillin
- pH
- Normally varies with systemic acid-base status
- PH should fall before 5.3 (usually below 5.0) with systemic metabolic acidosis
- Above 5.3 in adults and 5.6 in children indicate RTA
- PH goal 6.0-6.5
- Separate individual RTAs through FR of HCO3 at various serum HCO3 levels
- Also can monitor urine pH to look for success in treating metabolic alkalosis
- Look for pH > 7
- In treatment of uric acid stone disease
- Want to shift eq: H + urate – <=> uric acid to the left because urate is more soluble
- PH goal 6.0-6.5